Abstract
Background: Increased baseline white blood cell count (WBC) has been associated with vaso-occlusive complications in sickle cell disease (SCD), raising concern for the use of mobilizing agents that increase WBC count for hematopoietic progenitor cell (HPC) collection for gene therapy. Indeed, G-CSF, which predominantly increases neutrophil counts, when administered to SCD patients can precipitate life-threatening vaso-occlusion. Such vaso-occlusion, however, does not always correlate with degree of white blood cell count elevation (Fitzhugh C et al, Cytotherapy 2009) and G-CSF is associated with increases in neutrophil activation and adhesion. This raises the question whether WBC might be a surrogate for other proposed contributors to vaso-occlusion, such as activation of white cells, platelets, and coagulation. We examined this issue in the context of a clinical study of HPC mobilization with a single dose of plerixafor alone in clinically stable SCD patients.
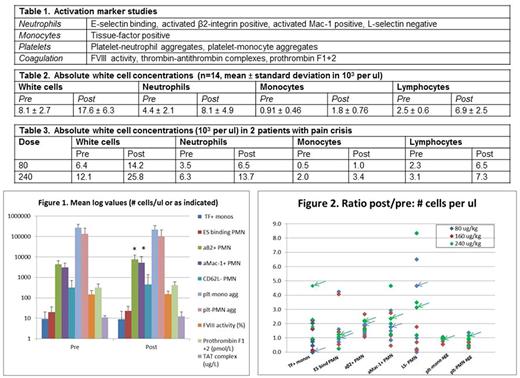
Materials and Methods: 14 patients (13 SS, 1 SB0, median age 31 with range 21-46) have completed the study so far (6 patients at 80 ug/kg, 3 patients at 160 ug/kg, and 5 patients at 240 ug/kg). 10 patients were on hydroxyurea (HU) at a median dose of 25 mg/kg (range 16-28 mg/kg) with a mean HbF of 17% versus 7% for the non-HU treated patients. Only one patient (non-HU treated) had received recent red cell transfusion (for leg ulcers) and had HbA (54%) present. Whole blood was collected at means of 4 hr pre-dose and 12 hr post-dose for activation marker studies by flow cytometry (cell studies) or ELISA (coagulation studies) as listed in Table 1.
Results: Increases in absolute total white cell, neutrophil, monocyte, and lymphocyte concentrations in whole blood with plerixafor treatment were all highly significant (Table 2, p < 0.002), without significant differences between HU- and non-HU treated patients or between dose levels. Twelve of 14 patients, however, did not experience any significant adverse events from plerixafor administration. Absolute neutrophil counts (ANC) were strongly correlated with absolute concentrations (but not percentages) of activated β2 integrin neutrophils (r= 1.0) and activated Mac-1 neutrophils (r= 0.8) but no other activation markers. We observed significant plerixafor-associated increases in activation markers (Figure 1) only for ANC subsets positive for activated β2 integrin (1.7± 0.44 fold, mean ± SD, p=0.002) and activated Mac-1 (1.7 ± 1.2 fold, p=0.05), which the correlations with ANC partly explain. The activated Mac-1 significance, however, disappeared with Bonferroni correction. There were no significant differences in activation markers between dose levels or between HU- and non-HU treated patients. There were moderate correlations between activated β2 integrin or activated Mac-1 and absolute reticulocyte count (r= 0.6 for both) and HbF (r= -0.5 for both) but not between these activation markers and LDH. Two patients had pain crises starting at 48 hr (80 ug/kg dose) and 81 hr (240 ug/kg dose) post-plerixafor administration; their pre and post-dose (12 hr) white counts are shown in Table 3. The fold-increase in activation markers for these 2 patients is summarized in Figure 2 (for each activation marker, color-coded arrows point to the two patients)
Conclusion: As with G-CSF, elevation of WBC or their subsets with plerixafor is not necessarily associated with vaso-occlusion, as manifested by pain crises. In our study, however, ANC elevation correlated with absolute concentrations of neutrophils positive for activated β2 integrin and activated Mac-1, which were the only activation markers significantly increased with plerixafor. These activation markers in turn correlated with reticulocyte count and HbF, which influence SCD vaso-occlusive severity. Vaso-occlusion as manifested by pain crises, however, was not consistently associated with the highest fold increases in ANC or activation markers. Therefore it remains unclear which bioassays correlate with vaso-occlusion associated with plerixafor mobilization.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal